
There has been a problem with Learn, please contact the administrator of the academy. Error code: 126692f2-e927-4bf7-b621-e4fd56a48320.
There has been a problem with Learn, please contact the administrator of the academy. Error code: 4b82b286-38b2-4212-9cdd-3b024873e7b9.
Learning Objectives
Why Risk Management Matters
Risk management in telemedicine is about identifying potential issues before they become problems. Whether it’s a technical glitch, operational hiccup, or reputational concern, a proactive approach minimizes disruption and safeguards patient care.
Learning Objectives
-
Understand what telemedicine entails and its inherent risks.
-
Recognize why early risk identification is crucial.
-
Develop a mindset for continuous monitoring and improvement.
Telemedicine and Risk Management
Understanding the Risks in Telemedicine
Unlike traditional healthcare settings, telemedicine relies heavily on digital platforms, remote communication, and electronic data storage, which expose physicians to unique security, compliance, and operational risks.
Common Telemedicine Risks
1. Cybersecurity and Data Breaches
- Unauthorized access to patient information
- Weak security protocols leading to HIPAA violations
- Cyberattacks such as phishing, malware, and ransomware
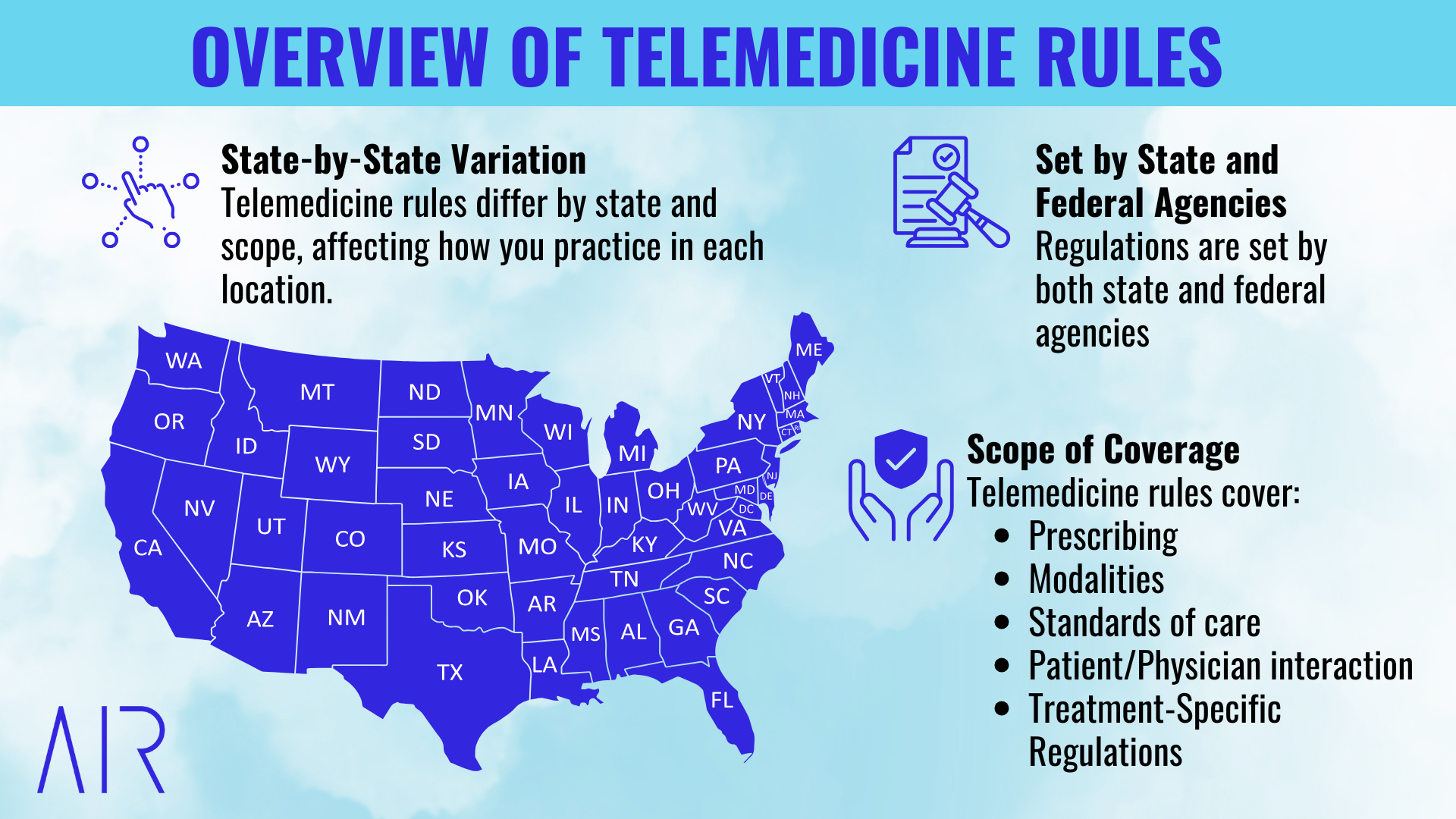
- Variations in state licensing laws and telehealth regulations
- Failure to meet HIPAA and HITECH security standards
- Inconsistent documentation or failure to obtain proper patient consent
- Incomplete clinical assessments due to limitations of virtual exams
- Misdiagnosis or delayed referrals for conditions that require in-person evaluation
- Medication errors due to unclear communication or lack of access to patient records
- Technology failures leading to missed or delayed appointments
- Overbooking and poor time management, leading to rushed visits and burnout
- Patient no-shows due to lack of clear instructions or technical difficulties
- Mental and physical fatigue from long hours of screen time
- Increased documentation workload without workflow automation
- Blurring of work-life boundaries, leading to stress and dissatisfaction
Recognizing Red Flags in Telemedicine
Telemedicine presents unique challenges in diagnosis, compliance, and patient interactions. Some red flags may be minor workflow inefficiencies, while others could pose serious legal or patient safety risks.
- Clinical Red Flags: When Virtual Care is Insufficient
Not all conditions can be safely managed via telemedicine. Some cases require in-person evaluation, imaging, or urgent intervention.
Common Clinical Red Flags:
- Unclear or unreliable patient-reported symptoms that require a physical exam
- Sudden onset of neurological symptoms (e.g., severe headache, unilateral weakness, slurred speech)
- Shortness of breath, chest pain, or signs of cardiovascular distress
- Severe abdominal pain with rebound tenderness or suspicion of surgical conditions
- Unexplained weight loss or persistent symptoms that raise concerns for malignancy
- Significant mental health crises (e.g., suicidal ideation, psychosis) requiring immediate intervention
- Pediatric patients with high fever, lethargy, or dehydration signs
How to Assess and Respond:
- Use structured clinical decision-making tools to determine if an in-person visit is needed.
- Ask detailed, guided questions to assess symptom severity and duration.
- Have a clear referral protocol for directing patients to urgent care, ER, or specialists when needed.
- Document your decision-making process and referral instructions to ensure liability protection.
- Follow up to confirm patient compliance with in-person referrals, if appropriate.
- Compliance Red Flags: Identifying and Addressing Regulatory Risks
Telemedicine is subject to state laws, prescribing regulations, and HIPAA requirements. Failing to comply can lead to legal consequences, fines, or loss of licensure.
Common Compliance Red Flags:
- Practicing across state lines without appropriate licensure or telehealth registration
- Prescribing controlled substances via telemedicine without confirming the state's rules
- Using non-HIPAA-compliant video conferencing or messaging platforms (e.g., standard Zoom, FaceTime, WhatsApp)
- Failure to document patient consent for telehealth services
- Not verifying patient identity before initiating consultations
- Billing for services not rendered or improperly coding telehealth visits
How to Assess and Respond:
- Regularly check state-specific licensing and prescribing laws through FSMB Telemedicine Policies.
- Use only HIPAA-compliant telemedicine platforms and avoid storing patient data on personal devices.
- Implement standardized telehealth consent forms and require identity verification before visits.
- Conduct periodic audits of billing, coding, and documentation to ensure compliance.
- If you discover non-compliance, self-report to legal counsel or compliance teams before authorities flag it.
- Operational Red Flags: Workflow and Technology Failures
Operational inefficiencies in telemedicine can disrupt patient care, increase liability risks, and reduce financial viability.
Common Operational Red Flags:
- Frequent appointment no-shows without a clear cancellation policy
- Technical issues disrupting patient care, such as poor internet connections or dropped calls
- Inconsistent documentation, missing key details needed for audits or malpractice protection
- Overbooking and provider fatigue, leading to rushed visits and potential clinical errors
- Patient complaints about miscommunication, long wait times, or billing issues
How to Assess and Respond:
- Implement automated reminders and cancellation policies to reduce no-shows.
- Use backup internet solutions (e.g., mobile hotspot, Ethernet connection) to prevent connectivity disruptions.
- Standardize SOAP note templates and use speech-to-text tools (e.g., Dragon Medical One) to improve documentation accuracy.
- Ensure realistic scheduling with buffer time between visits to prevent provider fatigue.
- Monitor patient satisfaction scores and address recurring complaints with workflow adjustments.
Handling Compliance Issues in Telemedicine
Even the most well-managed telemedicine practices encounter compliance challenges. Whether it’s an unintentional licensing violation, improper prescribing, a HIPAA breach, or billing errors, how a provider responds to compliance issues determines legal and professional consequences.
This guide provides a structured approach to identifying, addressing, and preventing compliance violations, along with examples of real-world scenarios to illustrate best practices.
Step 1: Assess the Severity of the Compliance Issue
When a compliance issue arises, the first step is determining its severity. Some violations may be minor and correctable, while others require immediate reporting to legal counsel, compliance officers, or state medical boards.
| Type of Compliance Issue | Examples | Risk Level |
|---|---|---|
| Minor Compliance Errors | Incorrect billing code used; missing but non-critical documentation; minor technical HIPAA violation (e.g., logging into telehealth software on a personal device) | Low – Correct internally |
| Regulatory Violations | Treating a patient without proper licensure in their state; prescribing medications without meeting legal requirements; using a non-HIPAA-compliant platform for patient communications | Moderate to High – Requires immediate correction |
| Serious Legal or Ethical Breaches | Failing to report a data breach; altering documentation after an issue has occurred; practicing without a valid medical license | High – May require self-reporting to regulatory bodies and legal involvement |
What Not to Do:
✖ Ignore a compliance issue or assume it won’t be noticed—many violations are caught in audits or patient complaints.
✖ Attempt to cover up errors by modifying patient records without notation—this is a legal red flag.
✖ Continue treating patients across state lines without verifying licensure—this can result in fines and revocation of licensure.
What to Do:
✔ Categorize the compliance issue (minor, moderate, or serious) before taking action.
✔ Consult legal or compliance experts before making corrective steps for high-risk violations.
✔ Act quickly—many regulatory bodies expect self-reporting and immediate mitigation.
Scenario: Licensing Violation (Regulatory Compliance Risk)
Dr. Smith, a New York-based telemedicine provider, consults a patient in Florida but does not hold a Florida medical license. He prescribes a routine medication without realizing Florida requires telemedicine-specific registration.
Compliance Risk Level: Moderate to High
Immediate Action:
- Dr. Smith immediately halts any further consultations with out-of-state patients.
- He notifies his legal and compliance team to assess potential penalties.
- The Florida Board of Medicine is contacted to determine next steps, which may include applying for licensure or paying a fine.
- His telemedicine group implements an automated patient location verification system to prevent future cross-state licensing issues.
Outcome: By self-reporting and taking immediate corrective steps, Dr. Smith minimizes potential penalties.
Step 2: Take Immediate Corrective Action
Once the severity of the issue is determined, take swift corrective action to mitigate risk. The response will vary depending on the type of compliance issue.
Corrective Actions by Issue Type
1. Licensing and Scope of Practice Violations
Common Mistakes:
- Providing care to patients in states where the provider is not licensed.
- Supervising mid-level providers (NPs, PAs) without proper authorization in certain states.
- Exceeding telemedicine scope of practice laws (e.g., prescribing certain controlled substances without meeting in-person requirements).
What to Do:
- Immediately stop treating patients in unlicensed states.
- Consult legal counsel to determine whether self-reporting is required.
- Apply for appropriate licensure or telemedicine waivers in required states.
- Implement real-time patient location tracking software to prevent future state-based violations.
2. HIPAA and Patient Privacy Violations
Common Mistakes:
- Using unapproved video conferencing platforms (e.g., FaceTime, standard Zoom).
- Sending patient information via non-encrypted email.
- Leaving PHI visible on shared computer screens.
What to Do:
- Immediately secure exposed data and notify internal compliance teams.
- Determine if the breach meets HIPAA’s "significant risk" criteria—if so, report it within 60 days to the HHS Office for Civil Rights.
- Educate staff on correct procedures and require training on HIPAA-compliant platforms.
3. Improper Prescribing Practices
Common Mistakes:
- Prescribing controlled substances without an in-person evaluation when required by law.
- Not checking state-specific prescribing regulations (e.g., mandatory PDMP checks before issuing certain medications).
- Failing to document a proper patient-provider relationship before issuing a prescription.
What to Do:
- Cancel the improper prescription immediately and contact the patient with next steps.
- Review the state’s prescribing laws and update protocols to ensure compliance.
- If necessary, report the error to the appropriate state board to avoid legal repercussions.
Scenario: HIPAA Violation (Patient Privacy Risk)
Dr. Patel accidentally sends a follow-up email with patient test results to the wrong patient, disclosing confidential health information. The patient reports the issue.
Compliance Risk Level: High
Immediate Action:
- Dr. Patel immediately contacts his compliance officer to assess reporting requirements.
- A formal disclosure and apology are sent to the affected patient.
- The privacy team documents the breach and submits a report as required by HIPAA.
- A mandatory training session is implemented to reinforce proper patient data handling.
Outcome: By properly documenting and addressing the breach, Dr. Patel minimizes liability and prevents future occurrences.
Step 3: Document Everything
Proper documentation is critical when handling compliance issues. Regulatory bodies expect to see a clear record of what happened, how it was addressed, and what changes were made to prevent recurrence.
Best Practices for Documentation:
✔ Record the issue, investigation process, and corrective action taken.
✔ Use clear, factual language—avoid subjective or defensive wording.
✔ Note all communications with compliance officers, legal counsel, or regulatory agencies.
✔ If patient care is involved, document patient communication and follow-ups.
✔ Retain compliance documentation for regulatory audits.
What Not to Do:
✖ Backdate or alter medical records without notation—this can be considered fraud.
✖ Fail to document corrective action—regulators require proof of compliance efforts.
✖ Ignore internal reporting procedures—issues should be logged even if resolved internally.
Preventing Future Compliance Issues
While responding to compliance issues is essential, preventing them from occurring is even more critical.
Strategies for Prevention:
-
Conduct routine compliance audits to identify vulnerabilities before they become violations.
-
Use automated systems to flag potential regulatory issues (e.g., location-based patient tracking for licensing compliance).
-
Implement regular provider training on telemedicine regulations, HIPAA compliance, and prescribing laws.
-
Stay updated on regulatory changes—telemedicine laws frequently evolve at the state and federal levels.
-
Create a culture of transparency where providers feel comfortable reporting compliance concerns before they escalate.
RESULT:
Approved
Your score:
Here are your results.
Congrats, you know your stuff!
RESULT:
Try Again
Your score:
Here are your results.
Please try again.
Knowledge Check
A knowledge check is a quick assessment designed to reinforce learning and gauge understanding of key concept.
Telemedicine Compliance Risk Self-Assessment
This self-assessment helps evaluate your compliance in key areas of telemedicine. Answer each question honestly to determine whether corrective actions are needed.
Licensing & State Regulations
❏ Am I licensed in every state where I see patients?
❏ Do I verify patient location before each visit?
❏ Have I checked whether my state requires additional telemedicine registration?
❏ If part of the Interstate Medical Licensure Compact (IMLC), am I tracking renewal deadlines?
Red Flag: Seeing patients in unlicensed states can lead to board investigations, fines, and disciplinary actions.
Fix It: Track your own licensure, and never assume the telehealth company ensures compliance.
HIPAA & Patient Privacy
❏ Do I only use HIPAA-compliant video platforms (not FaceTime or regular Zoom)?
❏ Is my computer encrypted and used only for telemedicine?
❏ Do I avoid storing patient notes on personal devices?
❏ Have I reviewed how to report a HIPAA breach if it occurs?
Red Flag: Sending patient information via personal email or text violates HIPAA and can result in major fines.
Fix It: Use only encrypted, HIPAA-compliant communication tools.
Prescribing & Medication Compliance
❏ Do I check state laws before prescribing controlled substances?
❏ Have I confirmed whether an in-person exam is required before prescribing?
❏ Do I review Prescription Drug Monitoring Programs (PDMPs) before issuing prescriptions?
❏ Is every prescription clearly documented to protect against audits?
Red Flag: Some states ban controlled substances via telemedicine, and violating these laws could result in loss of licensure.
Fix It: Never prescribe across state lines without verifying state-specific regulations.
Documentation & Medical Records Compliance
❏ Are all telemedicine visits documented with complete SOAP notes?
❏ Do I obtain and document patient consent for telehealth?
❏ Am I following state and federal medical record retention rules?
Red Flag: A missing patient consent form or incomplete SOAP note can make defending a malpractice claim difficult.
Fix It: Always document telemedicine encounters fully and store records properly.
Billing, Fraud, & Payment Compliance
❏ Am I using the correct CPT codes for telemedicine?
❏ Do I review claims to ensure services were billed accurately?
❏ Am I avoiding upcoding or billing for services I did not perform?
Red Flag: A telemedicine company bills services under your NPI without your knowledge, making you liable for fraud.
Fix It: Request regular claim reports to ensure no fraudulent billing occurs under your name.
Final Risk Summary
How many risks did you identify?
☐ None (Fully Compliant)
☐ 1-3 (Moderate Risk – Take Preventive Action)
☐ 4+ (High Risk – Immediate Corrective Steps Needed)
Next Steps: Address all moderate and high-risk areas to protect your license and remain compliant.
Telemedicine Compliance Corrective Action Plan (CAP) Template
This Corrective Action Plan (CAP) is designed to help address and resolve compliance risks in licensing, prescribing, HIPAA, documentation, and billing. Use this template to identify non-compliance issues, outline corrective steps, assign responsibilities, and track progress.
1. General Information
- Date of Corrective Action Plan Initiation: ________________________
- Person Responsible for Implementation: ________________________
- Department/Role (if applicable): ________________________
- Target Completion Date: ________________________
2. Compliance Issue Identified
-
Compliance Category:
☐ Licensing & State Regulations
☐ HIPAA & Patient Privacy
☐ Prescribing & Medication Compliance
☐ Documentation & Medical Records Compliance
☐ Billing & Payment Compliance
☐ Other: ________________________ -
Describe the Issue:
(Clearly explain the specific compliance issue, including what was identified, how it was discovered, and any consequences.) -
Risk Level Assessment:
☐ Low (Minor issue, corrective action needed but no immediate risk)
☐ Moderate (Compliance concern that needs urgent correction)
☐ High (Serious risk requiring immediate intervention to avoid penalties or loss of licensure)
3. Root Cause Analysis
-
What caused the compliance issue?
☐ Lack of awareness or training
☐ System failure (e.g., technical issue with telehealth platform)
☐ Human error (e.g., miscommunication, oversight)
☐ Policy/procedure gap
☐ Other: ________________________ -
Has this issue occurred before?
☐ Yes (Provide details: ___________________________)
☐ No -
Potential Impact if Left Unresolved:
☐ Legal penalties or medical board action
☐ HIPAA violation and patient privacy risks
☐ Patient harm or medication error
☐ Financial loss due to improper billing
☐ Other: ________________________
4. Corrective Actions & Implementation Plan
| Corrective Action Steps | Person Responsible | Due Date | Status |
|---|---|---|---|
| 1. Describe the first corrective action needed. | Name/Role | MM/DD/YYYY | ☐ Not Started ☐ In Progress ☐ Completed |
| 2. Describe the second corrective action needed. | Name/Role | MM/DD/YYYY | ☐ Not Started ☐ In Progress ☐ Completed |
| 3. Describe the third corrective action needed. | Name/Role | MM/DD/YYYY | ☐ Not Started ☐ In Progress ☐ Completed |
5. Monitoring & Follow-Up Plan
-
Who will ensure corrective actions are completed?
☐ Self-monitoring
☐ Compliance officer or legal counsel
☐ Telemedicine platform representative
☐ Other: ________________________ -
How will compliance be monitored after the corrective action is implemented?
☐ Internal audits or chart reviews
☐ Regular documentation checks
☐ Additional training or policy updates
☐ Technology improvements or automation
☐ Other: ________________________ -
Follow-Up Date for Review of Compliance Fix: ________________________
Telemedicine Company Evaluation Checklist
The Telemedicine Company Evaluation Checklist helps healthcare professionals assess telemedicine providers for compliance, reliability, security, and overall service quality.
AIR Launch Program Courses
Take charge of your own telemedicine journey. Explore other courses aimed to help you go even further.