
There has been a problem with Learn, please contact the administrator of the academy. Error code: 126692f2-e927-4bf7-b621-e4fd56a48320.
There has been a problem with Learn, please contact the administrator of the academy. Error code: 4b82b286-38b2-4212-9cdd-3b024873e7b9.
.png?width=1920&height=1080&name=JAN1%20AIR%20mentality%20(7).png)
Stepping into telemedicine is not just about learning new technology—it requires a fundamental shift in how you think, adapt, and operate as a physician. Whether you’re navigating new patient populations, multi-state licensing, or digital care models, success in telemedicine depends on your ability to assess situations, adapt to challenges, and take action with confidence.
This course is designed to help new telemedicine physicians develop a strategic approach to uncertainty, strengthen adaptability, and cultivate a resilient mindset—ensuring they not only survive but thrive in this evolving space.
Learning Objectives
By the end of this course, you will:
- Develop a framework for shifting your mindset from traditional in-person care to virtual practice.
- Learn to assess challenges effectively and make data-driven decisions in uncertain environments.
- Master key adaptability strategies to pivot, grow, and refine your approach in telemedicine.
- Strengthen resilience and confidence while handling setbacks or patient skepticism.
- Create a professional development plan for long-term success in virtual care.
Framework for Mindset Shifts
When physicians enter telemedicine, many feel unprepared, uncomfortable, and hesitant—which is completely normal. But the difference between success and frustration is how you handle that discomfort.
Instead of seeing challenges as roadblocks, shift your mindset to view them as part of the learning process. Every time you feel uncomfortable, you’re building a new skill, learning something valuable, and improving your ability to adapt.
Key Considerations
- Discomfort = Growth. If you feel unsure, that’s a sign that you’re stepping into new territory and expanding your abilities.
- Fixed vs. Growth Mindset. A fixed mindset says, “I’m just not good at this.” A growth mindset says, “I’m not good at this YET.”
- Experimenting is part of success. The best telemedicine physicians didn’t start out confident—they built confidence by trying, failing, and improving.
Takeaway: Instead of waiting to feel “ready” for telemedicine, start learning by doing. The best way to get comfortable is to get started.
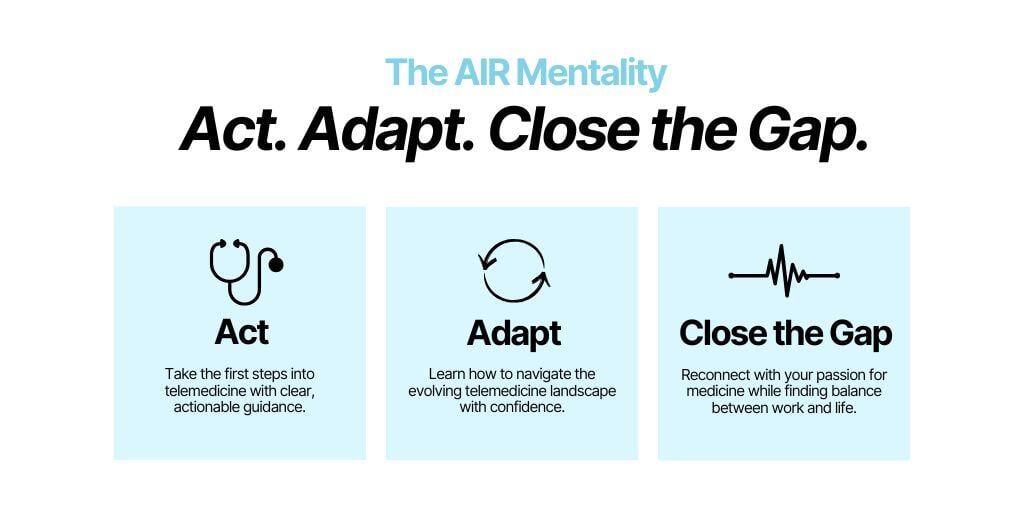
The AIR Mentality: Act, Adapt, Close the Gap
Many physicians hesitate in telemedicine because they’re waiting to feel fully prepared before taking action. But telemedicine moves fast, and success requires action, experimentation, and refinement.
The AIR Mentality is a framework to help you push past uncertainty and continuously improve:
Key Considerations
A – Act: Try Something Before You Feel Ready
- Confidence comes AFTER action, not before.
- Don’t overthink—try something, and learn from the experience.
- Take small steps: Start with one telehealth visit, one new tool, one adjustment.
I – Iterate: Learn from Each Experience
- Every visit, patient interaction, or workflow issue teaches you something.
- Ask: What worked? What didn’t? What can I tweak?
- Stay flexible and keep adjusting instead of getting stuck.
R – Refine: Improve Over Time
- Growth happens through small, consistent improvements.
- What seemed hard at first becomes second nature with practice.
- Seek feedback, refine your approach, and commit to learning as you go.
Takeaway: Waiting to feel fully prepared is a mistake. Take action now, learn from the process, and refine as you go.
Building Confidence and Resilience
Confidence isn’t about knowing everything—it’s about being comfortable with the process of figuring things out. The most confident telemedicine physicians are those who trust their ability to adapt, not those who have all the answers upfront.
Key Considerations
- You don’t need to be perfect to be effective. Patients don’t expect perfection—they expect competence, effort, and problem-solving.
- Confidence is a byproduct of experience. Every telemedicine visit makes you sharper, more efficient, and more comfortable.
- Resilience is key. There will be setbacks, mistakes, and moments of frustration—but pushing through them is what makes you stronger.
Strategies to Apply
- Normalize mistakes. Instead of avoiding them, use them as stepping stones for improvement.
- Reflect on small wins. Every time you handle a telehealth visit better than before, recognize your progress.
- Reframe failure. Instead of thinking, “I’m bad at telemedicine,” shift to “I’m learning how to get better.”
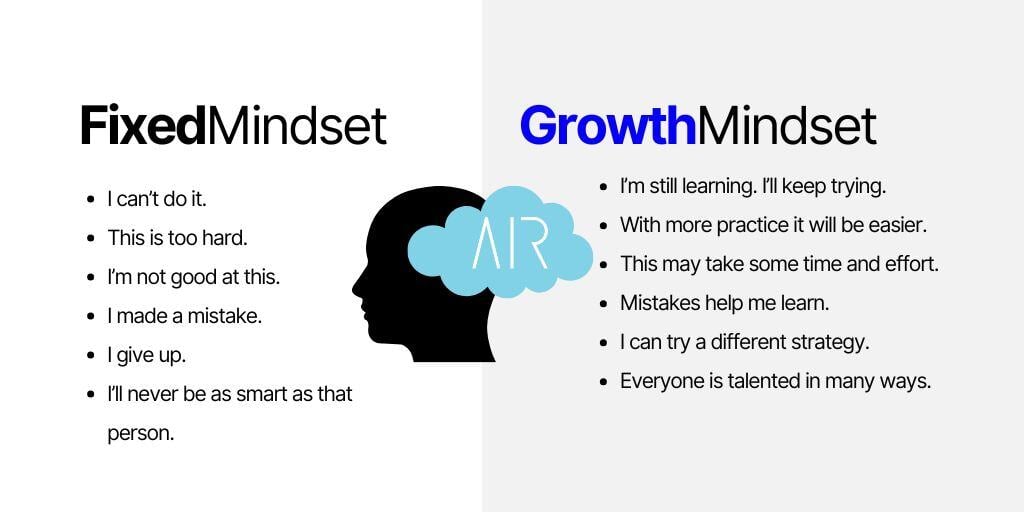
Growth Mindset in Action
A growth mindset is the belief that skills, knowledge, and confidence are built—not something you either have or don’t. Physicians who thrive in telemedicine are those who actively seek out learning opportunities and embrace the unknown.
Key Considerations
- The most successful physicians are lifelong learners. The ones who stay ahead are the ones who never stop improving.
- It’s okay to struggle at first. No one is good at something the first time they try it—what matters is persistence.
- Stay curious. When something doesn’t work, instead of getting frustrated, get interested. Ask what you can learn from it.
Strategies to Apply
- Ask “What can I learn from this?” instead of “Why is this happening?”
- Find mentors or colleagues who have been through similar challenges.
- Challenge yourself to try new things—new workflows, new technologies, new patient interactions.
Takeaway: Growth doesn’t happen by staying comfortable. Step into new challenges and embrace the learning process.
Motivation and Professional Development
Long-term success in telemedicine isn’t just about getting comfortable with virtual care—it’s about continuing to grow, adapt, and push yourself toward new challenges. The most fulfilled and successful telemedicine physicians stay engaged, continue learning, and actively seek opportunities for professional development.
Telemedicine is evolving rapidly. Physicians who invest in their own education, seek leadership roles, or explore new models of care will have more career mobility and stay ahead of industry changes. This means making learning a lifelong habit, setting clear goals, and consistently pushing yourself outside your comfort zone.
Key Considerations
Set Long-Term Goals for Your Growth
- What do you want your telemedicine career to look like in 6 months? 1 year? 5 years?
- Are you looking to specialize, take on leadership roles, or build expertise in new areas?
- The best opportunities go to those who position themselves as experts and thought leaders.
Stay Curious & Keep Learning
- Telemedicine is changing fast—staying engaged ensures you don’t get left behind.
- Be open to new business models, emerging technology, and evolving regulations.
- A commitment to learning makes you more adaptable, more valuable, and more resilient.
Prevent Burnout by Structuring Your Growth
- Balance clinical work with professional development—invest in learning, but don’t overload yourself.
- Take breaks, set boundaries, and schedule time for reflection and skill-building.
- Find mentors, peer networks, or professional groups to stay engaged.
Strategies to Apply
- Schedule dedicated time for ongoing education—whether that’s reading, attending webinars, or listening to industry leaders.
- Challenge yourself to take on something new—whether it’s leadership, education, system improvement, or exploring new models of care.
- Check in with yourself regularly: Are you still growing? Are you engaged in your own career evolution?
Books & Podcasts to Keep You Motivated & Growing
- Mindset: The New Psychology of Success – Carol S. Dweck
A foundational book on shifting to a growth mindset, learning from failures, and continuously improving. - Atomic Habits – James Clear
A powerful book on how small changes and consistent habits lead to long-term professional success. - The Obstacle Is the Way – Ryan Holiday
A guide to using challenges as opportunities for growth rather than roadblocks. - Range: Why Generalists Triumph in a Specialized World – David Epstein
Explores why physicians and professionals who develop broad, adaptable skills thrive in changing industries. - Podcast: The Knowledge Project – Shane Parrish
Discussions with top thinkers on decision-making, adaptability, and professional development. - Podcast: The Drive with Peter Attia
Deep insights into high-performance habits, professional resilience, and long-term career growth. - Podcast: HBR IdeaCast – Harvard Business Review
Features industry leaders discussing strategies for staying adaptable, resilient, and future-proofing your career.
Mindset Reflection
Before you can truly grow in telemedicine, you need to understand where you are now—what beliefs, fears, or habits might be helping or holding you back. This reflection will help you evaluate your mindset, identify areas for growth, and set clear, actionable goals.
Key Considerations
- How do you currently handle uncertainty? Do you see challenges as roadblocks or learning opportunities?
- Are you embracing discomfort, or are you avoiding it? Growth comes from stepping outside your comfort zone.
- Do you take action even when you feel unsure? Confidence is built by doing, not by waiting for certainty.
Reflection Questions to Apply
- What areas of telemedicine make me feel uncertain or hesitant?
- How do I typically react when I don’t have all the answers?
- What’s one belief I need to shift to become more adaptable and confident in this space?
- What’s one small action I can take this week to step into discomfort and grow?
Takeaway: Growth starts with self-awareness. Before you can improve, you need to recognize where you are now and what you need to work on.
Self-Assessment Checklist
This checklist helps you assess where you stand in your growth mindset, adaptability, and professional development. It’s designed to highlight strengths and areas where you can push yourself further.
Growth Mindset & Adaptability Checklist
Mindset for Learning & Growth:- I am open to learning and trying new approaches in telemedicine.
- I see challenges as opportunities for growth, not as failures.
- I am willing to adjust my strategies if something isn’t working.
- I take action even when I don’t feel 100% ready.
- I am comfortable making decisions with limited information.
- I handle patient and system challenges with a problem-solving mindset.
- I dedicate time for ongoing education, books, podcasts, or courses.
- I set long-term career goals and check in on my progress regularly.
- I actively seek feedback to improve my telemedicine skills.
Takeaway: If you checked all or most boxes, you’re already embracing a growth mindset. If not, identify 1–2 areas where you can challenge yourself to grow.
Reframing Challenges
Step 1: Identify a Challenge
What is one telemedicine challenge that makes you feel uncertain or uncomfortable?
(Example: “I don’t feel confident managing a virtual patient visit when technology fails.”)
Step 2: Reframe It as an Opportunity
What can you learn from this challenge? How can it make you better?
(Example: “Handling tech failures well will help me become more resilient and adaptable.”)
Step 3: Create a Plan of Action
What small step can you take to get better in this area?
(Example: “Practice troubleshooting common telemedicine tech issues so I feel more prepared.”)
💡 Takeaway: Instead of seeing challenges as obstacles, train yourself to see them as stepping stones for growth.
Confidence-Building Plan
Step 1: Identify a Growth Area
What’s one area where you feel uncertain or need more confidence in telemedicine?
Step 2: Develop an Action Plan
What’s one thing you can do this week to build confidence in this area?
(Example: “I will run a mock telemedicine session with a colleague to practice my virtual presence.”)
Step 3: Track Your Progress
At the end of the week, reflect: Did you improve? What worked? What needs more adjustment?
Takeaway: Confidence isn’t something you wait for—it’s something you build by taking action.
Physician Adoption of Telemedicine
Diel S, Doctor E, Reith R, Buck C, Eymann T. Examining supporting and constraining factors of physicians’ acceptance of telemedical online consultations: A survey study. BMC Health Services Research. 2023.
Key Takeaways:- Physician adoption of telemedicine is driven by usability, workflow efficiency, and reimbursement clarity.
- Top barriers include lack of familiarity, regulatory confusion, and technology resistance.
- Supportive policies, training, and easy-to-use platforms increase physician acceptance.
Miner H, Fatehi A, Ring D, Reichenberg JS. Clinician telemedicine perceptions during the COVID-19 pandemic. Telemedicine Journal and e-Health. 2020.
Key Takeaways:- The rapid shift to telemedicine during COVID-19 accelerated physician acceptance, but highlighted gaps in workflow adaptation and virtual communication skills.
- Many clinicians reported initial discomfort with virtual care but improved confidence over time.
- Long-term success in telemedicine requires training in virtual patient engagement, documentation, and compliance.
Clinician Behaviors in Telehealth & Best Practices
Henry BW, Block DE, Ciesla JR, McGowan BA, Vozenilek JA. Clinician behaviors in telehealth care delivery: A systematic review. Advances in Health Sciences Education. 2016.
- Key Takeaways:
- Virtual bedside manner is crucial. Non-verbal cues (eye contact, tone, body language) impact patient trust.
- Structured communication frameworks improve efficiency and patient satisfaction.
- Physicians need training in handling difficult patient interactions in a virtual setting.
Keyserling K, Janetos E, Sprague C. Teaching Telehealth During a Pandemic and Beyond: An Intern’s Survival Guide for Virtual Medicine. Journal of General Internal Medicine. 2021.
- Key Takeaways:
- New physicians often struggle with the transition to virtual care, requiring structured onboarding and mentorship.
- Checklists and pre-visit preparation improve telehealth visit flow and reduce stress.
- Physicians who embrace a growth mindset and seek continuous feedback improve faster in telemedicine.
Growth Mindset & Learning in Medicine
Hopkins SR, Rae VI, Smith SE, Tallentire VR. Trainee growth vs. fixed mindset in clinical learning environments: Enhancing, hindering, and Goldilocks factors. BMC Medical Education. 2024.
- Key Takeaways:
- Physicians with a growth mindset adapt faster to new clinical environments, including telemedicine.
- Fear of making mistakes hinders learning, while those who see challenges as learning opportunities improve faster.
- Structured reflection and feedback loops help physicians refine skills and build confidence.
Physician Well-Being & Burnout Prevention
Malik H, Annabi CA. The impact of mindfulness practice on physician burnout: A scoping review. Frontiers in Psychology. 2022.
- Key Takeaways:
- Mindfulness strategies significantly reduce burnout and improve focus during virtual visits.
- Physicians who engage in short, daily mindfulness exercises report higher resilience and better patient interactions.
- Telemedicine physicians should incorporate brief stress-reduction techniques to maintain focus and well-being.
How to Apply This Research to Your Practice
For telemedicine adoption & workflow efficiency:- Implement structured pre-visit checklists to streamline virtual consultations.
- Seek mentorship or training in virtual patient engagement if telemedicine still feels unfamiliar.
- Choose user-friendly telehealth platforms that integrate well with clinical workflows.
- Reframe mistakes as learning opportunities instead of setbacks.
- Engage in structured reflection to refine skills after each telemedicine session.
- Seek peer feedback or mentorship to accelerate learning and confidence-building.
- Use short mindfulness or reflection exercises before and after patient visits.
- Establish clear work boundaries to separate clinical time from personal time.
- Stay engaged in professional development to keep career motivation high.
Takeaway: These evidence-based insights provide practical guidance for improving telemedicine workflows, patient interactions, physician mindset, and long-term career sustainability.
Next Step: Choose one research-backed strategy to implement in your practice this week, whether it’s improving virtual communication, embracing a growth mindset, or refining workflows.
Personal SWOT Analysis
A Personal SWOT Analysis is a strategic tool that helps individuals identify their internal strengths and weaknesses alongside external opportunities and threats. This self-assessment empowers you to leverage your strengths, address areas for improvement, capitalize on opportunities, and mitigate potential challenges for personal and professional growth.Communication Techniques
Communication techniques encompass the various methods and strategies used to effectively convey ideas, emotions, and information between individuals or groups. They range from verbal and nonverbal cues to active listening and empathetic engagement, all of which are essential for fostering understanding and building strong relationships in both personal and professional settings.
Action Plan Template
An Action Plan Template is a structured document that outlines specific steps, responsibilities, and timelines to achieve a goal or complete a project efficiently. It helps track progress, allocate resources, and ensure accountability for successful execution.
Physician Adoption of Telemedicine
AIR Launch Program Courses
Take charge of your own telemedicine journey. Explore other courses aimed to help you go even further.